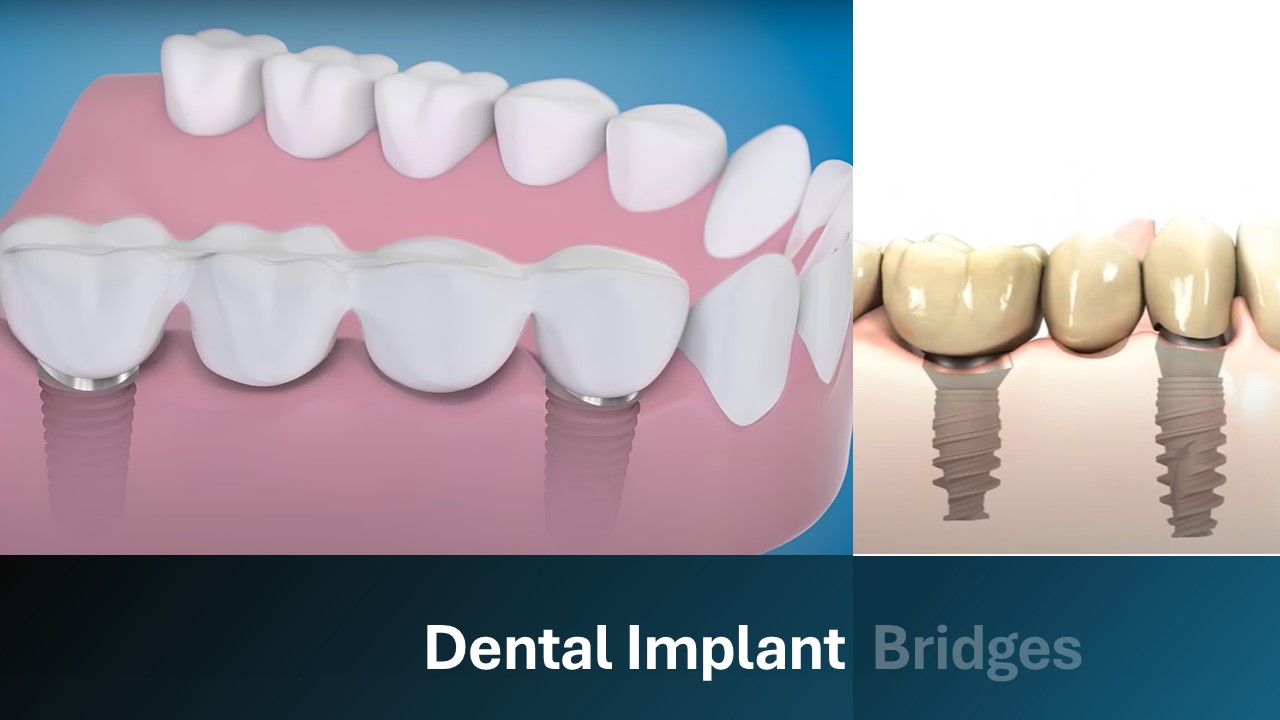
Dental implant-supported bridges are fixed prosthetics designed to replacemultiple missing teeth by anchoring onto dental implants surgically placed into the jawbone. Unlike traditional bridges that rely on adjacent natural teeth for support, implant-supported bridges are secured directly into the bone, offering enhanced stability and longevity. This approach not only restores the missing teeth but also helps maintain jawbone density, preventing the bone loss that typically follows tooth extraction.
Additionally, when aesthetic considerations make side-by-side implant placement impractical, implant-supported bridges step in to fill the void. Placing implants side by side may cause aesthetic problems, as a distance of at least 3 mm should be left between two implants in aesthetic areas. This distance can prevent the natural formation of the gingival papilla and negatively affect the appearance. Because of this, dental implant-supported bridges are typically the way to go for the front areas.
How do implant-supported bridges work?
Implant bridges are basically based on prosthetic teeth placed between implants. These bridges can be made of a single tooth or a bridge consisting of two teeth. There are also applications in the form of two teeth on a single implant, especially in areas where there is not enough space for Implant Bridge construction, especially in the back teeth.
In implant bridge treatments, implants are surgically inserted into the jawbone, where they fuse with the bone tissue through a process called osseointegration. This integration provides a solid foundation for the dental bridge, which is custom-made to match the patient's natural teeth in color, shape, and size.
Benefits of Implant-Supported Bridges
Implant bridges are targeted therapies and so necessitate only localized procedures. These treatments offer numerous advantages.
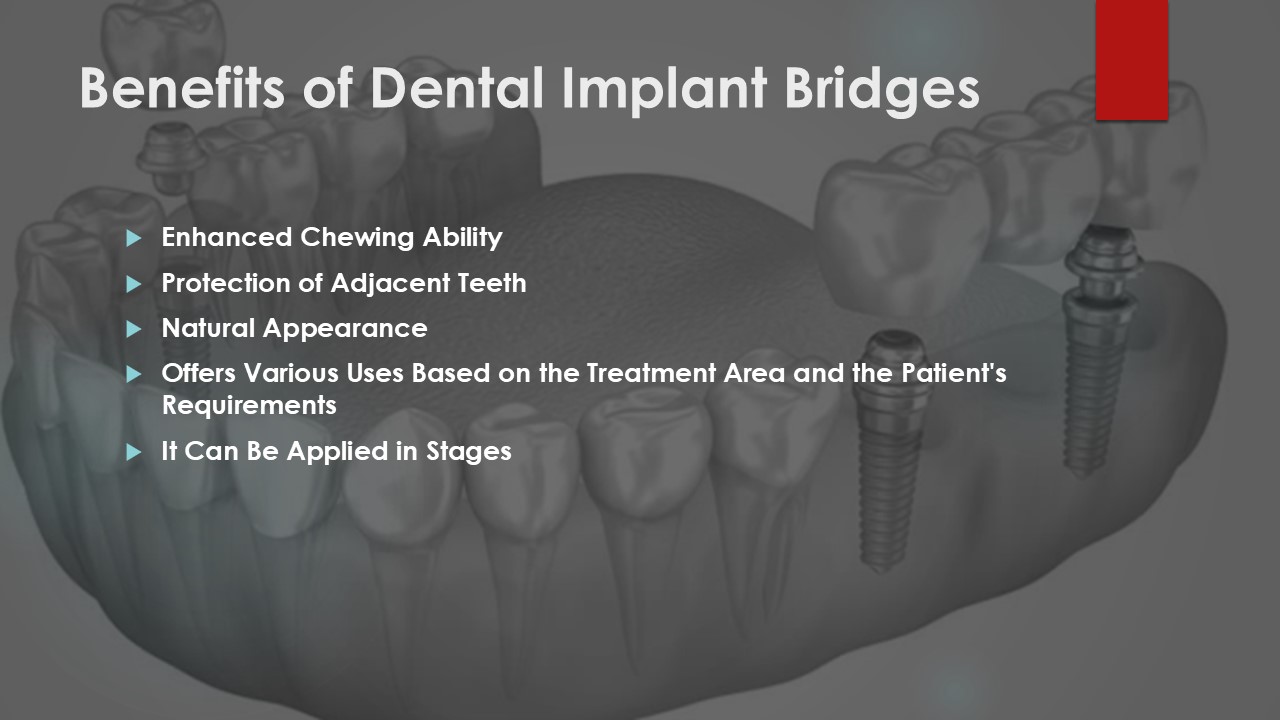
Enhanced Chewing Ability
Implant bridges provide a comfortable chewing experience because they distribute the load between the two implants during chewing. According to a study published in the International Journal of Oral & Maxillofacial Implants (Rangert et al., 1995), prostheses supported by the natural tooth and implant together were found to share the loads and the load on the implant remained below the limits. In the study, the vertical loads were shared evenly between the tooth and the implant, and the maximum bending moment on the implant was below the mechanical limits. The flexibility of the implant screw in adapting to the periodontal ligament of the natural tooth made load sharing possible.
Protection of Adjacent Teeth
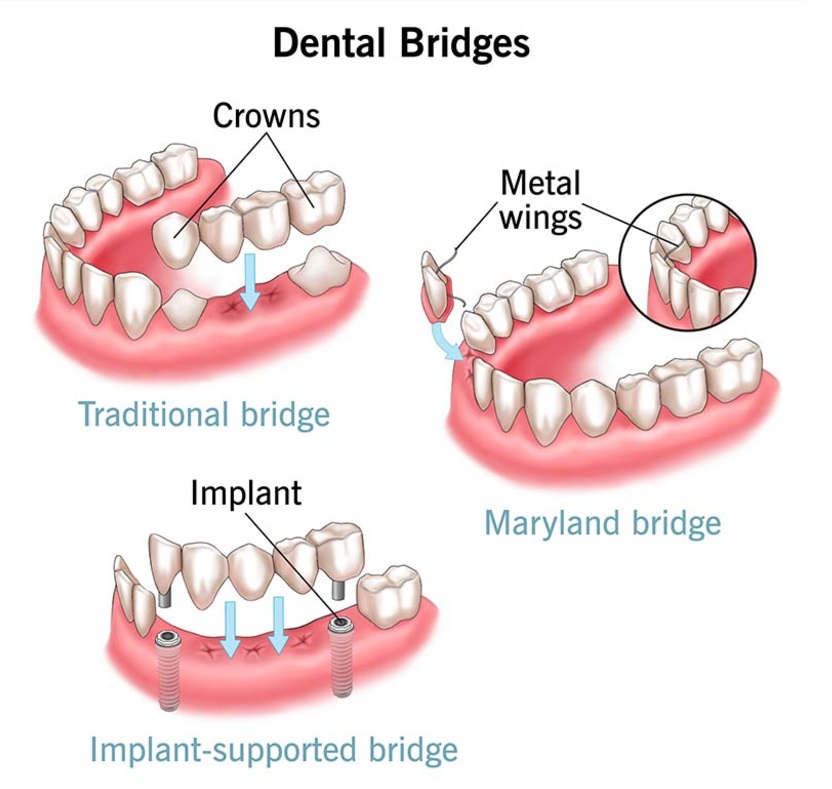
When placing a traditional bridge, it is necessary to grind down neighboring healthy teeth so that the prosthetic can fit into the space. With implant-supported bridges, this is no longer necessary, and the original teeth are protected from damage and decay.
Natural Appearance
Dentists have the freedom to tailor their management of implant bridge applications to each individual patient. On the other hand, there are treatments where dentists just do not have enough control over the cosmetic and functional aspects to guarantee high-quality results.
The All on Four procedure, for instance, has a laundry list of requirements that the dentist must adhere to. example: the treatment can't go further unless the patient gets a big bone graph extracted from their mouth and undergoes pink aesthetics.
As a regional treatment, implant bridges allow patients to have natural gums without the need for pink aesthetics—as long as there is sufficient bone and gum tissue in the affected location. With this, there is a significant improvement in visual appeal.
Offers various uses based on the treatment area and the patient's requirements.
Depending on the patient's condition and existing dental work, a variety of implant-supported bridge options are available. The modest size of the lower front teeth's construction means that the bone around them is often smaller as well. So, it could be required to remove some bone in order to create an adequate area for the implants. Although it is not always necessary, this procedure is usually necessary for cases involving the lower jaw.
On the other hand, In the maxilla, in uppeer jaw, the use of pink color for dentures is often discouraged. In certain instances, a pink prosthesis may be requisite; this is contingent upon the patient's individual requirements and treatment strategy.
It can be applied in stages
Placement of implant-supported bridges can be done in stages. When using this technique, healthy teeth are left alone during the first surgery while the remaining implants are inserted during the second procedure. Staging the placement of dental implants ensures that healthy teeth can be used to secure temporary prostheses, protecting both the bone and soft tissues from harmful consequences. Reduced reliance on short-term prosthesis also benefits bone and tissue health over time.
The Dental Implant Bridge Procedure
The first step in getting a dental implant supported bridge is a thorough exam. This procedure involves reviewing the patient's medical history and conducting imaging tests like X-rays or CBCT. Subsequently, a patient-specific therapy strategy is developed. While the patient is under local anesthesia, the surgeon places the implants in the jawbone and then closes the jaw to allow the tissue to heal.
Bone and implant typically merge during the healing phase, which can take anywhere from three to six months. You may keep your smile looking good and feeling great with temporary dentures while you wait. After the implants have healed, abutments are used to join them, and an imprint is made for the dental bridge. The bridge is fine-tuned and then permanently fastened once it is completed.
Candidates for Implant-Supported Bridges
Adequate Bone Density
The stability of dental implants relies on their robust integration into the jawbone. Implants integrate with the jawbone via osseointegration. However, without appropriate bone density, implant attachment becomes problematic and the chance of failure increases.
Periodontal disease or bone resorption following tooth loss can complicate implant installation. In this instance, adjunctive surgical interventions such as bone grafting are conducted. Furthermore, shrinking of the jawbone or lower jaw height complicates the implantation process.
Healthy Mouth and Gums
Maintaining good gum health is essential for the success of dental implants. Furthermore, periodontal diseases can cause inflammation in the tissues surrounding the implant, thereby compromising its stability.
Specifically, this condition, known as "peri-implantitis," may lead to the loss of the implant. Research indicates that individuals with a history of periodontal disease experience a 10-20% higher rate of implant failure. Consequently, it is imperative to address and treat gum diseases thoroughly before proceeding with the implant procedure.
General Health Status
Your overall health significantly influences both the speed of your recovery and the success of the implant integration. For instance, uncontrolled diabetes and other chronic conditions can impede the healing process. Specifically, high blood sugar levels not only slow down osteointegration but also increase the risk of infection.
Additionally, patients with certain blood abnormalities, such as clotting disorders, are more likely to experience bleeding after surgery. According to a study implant failure was 15% more common among individuals whose diabetes was not well-controlled. Therefore, managing chronic health conditions effectively is crucial for the successful outcome of dental implant procedures.
Lifestyle Factors
Smoking and heavy alcohol intake significantly impair the efficacy of dental implants. For example, smoking impedes wound healing by diminishing blood circulation in the oral cavity. Moreover, it hinders the osseointegration process and elevates the risk of peri-implantitis. As a result, the implant failure rate in smokers may reach up to 20%.
Similarly, alcohol consumption compromises the immune system, increases the risk of infection, and adversely impacts bone density. Consequently, individuals who smoke or consume alcohol heavily face greater challenges in achieving successful implant outcomes. Therefore, addressing these lifestyle factors is essential for optimizing the success rates of dental implants.
Implant-Supported Bridges Care and Maintenance
If you require an implant-supported bridge and it isn't because of a serious condition like diabetes, dry mouth, or pimples, you most likely need this treatment since you haven't been taking proper care of your teeth. Having said that, you will not receive the intended unit and result from any treatment if you do not make enough progress in improving your dental hygiene practices.
Periodontal diseases can have an impact on dental implants, just like they can with natural teeth. Attacks by oral bacteria on the implant roots result in the implant roots being exposed, trembling, and failing. This is the main cause of treatment failures. Below, we have provided a list of some post-bridge care instructions that are based on the scientific data. Be mindful to follow these instructions to the letter if you would prefer not to undergo these difficult treatments again.
Daily Oral Hygiene:
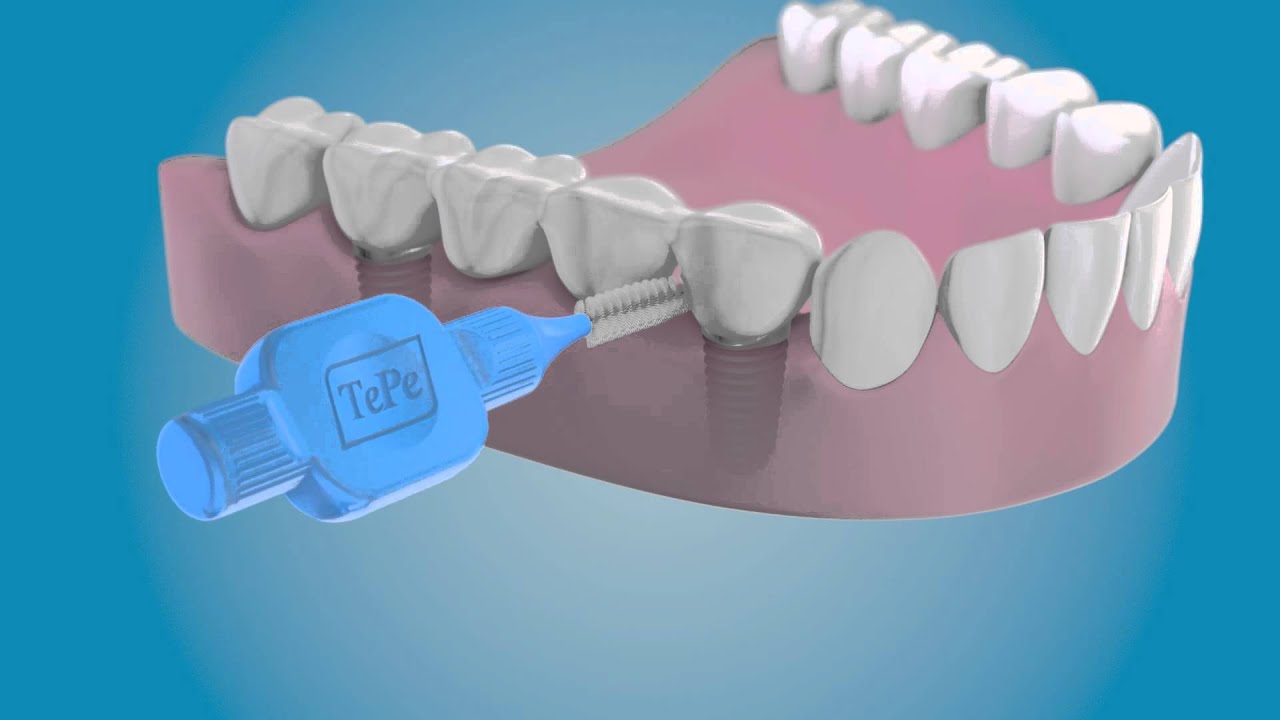
In 2011, 3 American dentists published a scientific article that states. "Personal oral hygiene must begin at the time of dental implant placement and should be modified using various adjuctive aids for oral hygiene to effectively clean the altered morphology of the periimplant region before, during and after implant placement. For instance, interproximal brushes can penetrate up to 3mm into a gingival sulcus or pocket and may effectively clean the peri-implant sulcus11"
The study also found that mouthwashes containing chlorhexidine have been shown in several studies to reduce the risk of peri-implantitis (Kurtzman and Silverstein, 2007).
Professional Cleaning and Monitoring:
Regular cleaning of the tissues around the implant by a dentist helps to detect infections early and prevent complications such as peri-implantitis.
Importance of Regular Check-ups:

Regular check-ups of implants allow early detection of problems such as bone loss or loosening. For the first year following implant placement, Dr. Gregori M. Kurtzman advises in his paper that every three months. It is emphasized that if the peri-implant tissues are healthy, this interval can be increased to 4-6 months.
A 2020 scientific study found that home toothpastes, especially fluoride-containing gel formulations, left more residue on the smooth surfaces of titanium than mouthwashes. It is stated that the longer these products stay on the surface, the more effective they may be in plaque control. Manual and electric toothbrushes, flossing, and interface brushes have also been reported to be useful in maintaining peri-implant health.
Dental Implant Supported Bridges Cost and Financing Options
Private insurance typically does not cover the higher cost of implant-supported bridges compared to regular bridges. Dental insurance often only pays for a portion of the cost of an implant and its repair, such as a bridge, and not the actual surgery to place the implant.
Although dental implant bridges are more expensive, the benefits they provide patients outweigh the cost. The aesthetics of the patient's jaw are greatly improved by the implants that are attached to the jawbone using implant-supported bridges. Furthermore, there is a way to significantly halt jawbone bone resorption. On the other hand, conventional bridges that does not include implants cannot provide the same cosmetic advantages.
Risks and Complications
Problems with impalant-supported bridge applications can arise from a number of sources, including inaccurate evaluations, measurements, or post-treatment lack of proper mouth hygiene. Here are a few of the issues that can arise:
Infection
Infections at the implant site can arise from a variety of sources. Among these, bacteria can grow in the region if the dentist doesn't clean the adhesive remnants thoroughly after the procedure.
Another factor is the possibility of infection at the implant site due to bone resorption that persists in the patient following therapy. The bridge and implant can come loose due to the buildup of bacteria and plaque around the implant, which can rip the connective tissue between the implant and the gums.
Implant Failure
The success rate of implant therapies is exceptionally high. Technical problems account for 60-80% of implant failures, whereas biological factors contribute to 40-60%, according to a scholarly report that analyzed 159 studies. Specifically, the study identified both biological and technical factors that influence implant success as follows.
Biological Complications (Body Related Problems):
- Peri-implant Mucositis: Inflammation of the soft tissues around the implant.
- Peri-implantitis: More severe inflammation leading to bone loss.
- Failure of Bone Integration: Failure to properly attach the implant to the bone.
- Infections: Problems caused by microbial contamination at the implant site.
- Allergic or Systemic Reactions: Rare allergic responses to the implant material.
Technical Complications (Mechanical Problems):
- Screw Loosening: Destabilization of the prosthesis due to loosening of the implant attachment screw.
- Screw Breakage: Breakage of screws due to overload or mechanical strain.
- Prosthetic Part Damage: Fracture of prosthetic structures such as crowns or bridges.
- Implant Fracture: Implant fracture due to mechanical loading or manufacturing defects.
- Compatibility Problems: Functional or aesthetic problems as a result of the prosthesis not being fully compatible with the implant.
Damage to the Nerves
During the implantation of dental implants can lead to issues such as numbness, tingling, discomfort, or permanent loss of sensation. Specifically, the nerves involved include the inferior alveolar nerve, which traverses the mandibular canal in the mandible and supplies sensation to the lower teeth, lower lip, and chin.
To mitigate the risk of nerve damage, it is essential to determine the location of the nerve pathways using imaging techniques such as panoramic x-rays or cone beam computed tomography (CBCT) prior to surgery. Additionally, surgical planning must be executed with precision. Employing meticulous surgical methods is crucial in reducing the likelihood of nerve injury during implant insertion. Furthermore, effective planning and implementation can significantly lessen the probability of this severe yet preventable consequence.
Mitigating Risks
Leverage Antlara Dental's two decades of expertise to mitigate hazards associated with dental implant procedures. Our dentists, possessing over 30 years of experience, can offer optimal treatment alternatives, while you can undergo a risk-free bridge procedure utilizing our advanced imaging technology.
FAQs
Below you will find the most frequently asked questions and answers about dental implants.
What Is the Difference Between a Tradational Dental Bridge and an Implant Bridge?
Conventional implant-supported bridges entail the construction of a third bridge tooth anchored by two natural teeth in implant-supported bridges, a bridge tooth is put between 2 implants. For dental implant-supported bridges, at least 3 teeth must be lost side by side. however, it is a less invasive procedure compared to older methods because it is applied without hurting nearby teeth.
How Long Do Dental Implant-Supported Bridges Last?
Unless there is a major error in the application and the patient experiences bone resorption or other issues that impact the implant's health, an implant-supported bridge is anticipated to endure for 20 to 25 years. The durability of bridge treatments, however, is heavily dependent on the implant's quality.
The use of substandard implants results in a significant proportion of patients requiring implant replacements. If you want your implant therapy to survive, it's crucial to use items from reputable firms like Straumann Nobel bio care. These products have been confirmed to be high-quality using scientific data, and the implant kinds they employ have been successful for nearly 30 years.
Is the Procedure Painful?
In most cases, local anesthetic is used to execute the painless procedure of bridge applications. On the other hand, general anesthesia is an option for patients with a high fear threshold.
How Do I Care for My Dental Implant Bridge?
For maintenance, you will need to get dental floss and toothbrushes specially developed for implant bridges. Standard toothbrushes may be inadequate for cleaning the areas under bridges. For this reason, interdental brushes that are thin and flexible enough to reach under bridges or special brushes up to 0.3 mm thick should be preferred.
Can Anyone Get a Dental Implant Bridge?
Yes, implant-supported bridges are appropriate for nearly everyone. If your bone density is insufficient, implants can be used to increase your bone density through bone augmentation procedures. However, implant treatments are not recommended for patients with blood coagulation issues or cancer.
Additionally, diabetes poses a danger because it hinders wound healing; however, patients with well-controlled diabetes can typically undergo implant treatment without incident. Another potential obstacle to implants is severe osteoporosis damaging the jawbone.
How Much Does a Dental Implant Bridge Cost?
In the United States, the average cost of a single arch implant bridge ranges from $4,000 to $15,000. If more implants are needed or if premium materials are chosen, this cost could go up.
The price range in European countries is 3,500 to 10,000 EUR. On the other hand, Poland and Hungary offer more reasonable prices.
Turkey, in contrast, stands out as a destination that provides dental implant therapy at an inexpensive price without sacrificing quality. Here is how costs can be assessed:
Costs between $350 and $1,000 for a single tooth implant.
Price range: $2,000 to $5,000 USD for a dental implant bridge (arch/arch).
Does Insurance Cover Dental Implant Bridges?
The majority of insurance policies will pay for a traditional bridge, but only a portion of the cost of an implant-supported bridge.
How Long Is the Recovery Time?
Implant-supported bridges, just like an implant treatment, require 3 to 6 months for the implant to fuse to the jawbone.
Are Implant-Supported Bridges Removable?
No patient should ever remove a fixed implant bridge. Some alternatives allow you to remove them for cleaning, including implant-supported overdentures.
What If I Don't Have Enough Bone Density?
Procedures such as bone grafting or sinus lifts can enhance bone volume, facilitating implant implantation. These supplementary treatments may prolong the total duration.
How Soon After Tooth Extraction Can I Get an Implant?
After the tooth is transplanted, a few weeks should pass for the implant to be healthy. There is a danger of infection during implant treatment if the wound does not heal properly during this time, or the wound may enlarge while treatment is underway, creating an ideal environment for plaque and bacteria to accumulate.
Will My Implant Bridge Look Natural?
The use of porcelain gums, or pink aesthetics, is unnecessary in implant-supported bridges when the patient's bone density is enough. Thus, the patient looks to have fully normal gums. For this reason above all others, bridge applications look so natural.
Do Dental Implants Require Special Care?
To keep dental implants in good condition, brush them regularly. To get beneath bridges, though, you need an extremely tiny interdental toothbrush that was made specifically for the purpose.
Can Smoking Affect My Dental Implants?
Smoking has serious negative effects on implants and is considered one of the most important causes of implant failures. For instance, a scientific study conducted on the effects of smoking on implants states that "in smokers, a higher failure rate and complications have been observed after dental implantation and related surgical procedures."
Moreover, the risk of failure and complications decreases once smoking is stopped. Consequently, potential implant patients should be warned that smoking could have a detrimental effect on dental implantation and the surgical procedures related to implants.
Is Age a Factor in Getting Dental Implants?
In the case of dental implants, age plays no role. Patients of any age can have implants placed if their bone density is adequate to hold them in place.
What Are the Success Rates of Dental Implants?
The success rate of dental implants is over 95%. However, this success rate is the average success rate in healthy individuals and individuals who pay attention to oral hygiene.
According to a study published in the Journal of Dental Research (Pjetursson et al., 2008), implant-supported bridges have a high success rate and patient satisfaction, making them a reliable long-term solution for multiple missing teeth.
- Conventional tooth-supported FDPs (Fixed Dental Prostheses): 93.8
- Implant-supported FDPs only: %95.2
- Combined FDPs with tooth-implant support: %95.5
- Implant-supported SCs (Single Crowns): 94.5
10-Year Survival Rates:
- Conventional FDPs: %89.2
- Implant-supported FDPs: %86.7
- Combined FDPs: %77.8
- Implant-supported SCs: %89.4
Complication Rates (After 5 Years):
- Implant-supported FDPs: %38.7
- Conventional FDPs %15.7
Can I Replace All My Teeth with Implant Bridges?
Without a doubt, implant bridges can replace all of your teeth. At our clinic, we suggest the phased therapy technique for this. This allows us to attach the bridge with minimal injury from the temporary prosthesis.
Are There Alternatives to Dental Implant Bridges?
Alternatives include traditional bridges and removable dentures. However, these may not offer the same stability, function, or bone preservation benefits as implants. However, you can also consider All on four and all on six for full mouth restoration.
How Do Dental Implants Impact Jawbone Health?
In the same way that real tooth roots stimulate the jawbone, dental implants do the same, stopping bone resorption and keeping the face in its natural shape.
What Is Peri-Implantitis and How Can It Be Prevented?
Peri-implantitis is an infection and inflammation of the gum and bone around an implant. It can lead to bone loss and implant failure. Prevention involves meticulous oral hygiene and regular dental check-ups.
How Does Bone Grafting Work?
Bone grafting is a procedure used to increase the volume and density of the jawbone. It is performed in cases where there is insufficient bone before implant placement. The bone material used can come from the following sources:
- Autocraft (patient's own bone): It has the highest success rate.
- Allograft (Donor bone): Bone material taken from another human being.
- Synthetic Materials: Artificially produced bone-like materials.
This allows the bone material to fuse with the jawbone, creating the solid structure necessary to support the dental implant.
Is the Implant Procedure Safe?
Dental implant surgery, in the hands of an experienced expert, poses no significant risk to the patient. Prior to the treatment, thorough analysis is carried out using panoramic x-rays and tomography to identify important characteristics, including bone structure and nerve connections. For the treatment to go off without a hitch, this is vital.
Surgical protocols are strictly followed and sterile conditions are maintained during the operation. All of these measures, when taken along with careful preparation and the assistance of a skilled team, guarantee the long-term reliability and effectiveness of implant treatment.
Conclusion
For extensive tooth loss, a therapeutic option that stands out is a dental implant bridge, which offers both immediate and long-term benefits. One major advantage of these treatments is that they do not harm natural teeth in any way.
However there must be meticulous attention to detail and the utilization of state-of-the-art imaging equipment during the entire implant-supported bridge application process. Thanks to the stunning outcomes it produces, we at Antlara Dental place a premium on this procedure and do our best to incorporate implant-supported bridges into our patients' treatment plans.
